- Home
- Symptoms Explainer
- Joint Pain
The Systemic Roots of Joint Pain
Joint pain is not merely a mechanical issue of cartilage wearing down, it is often a systemic signal of deeper biological stress. Emerging research on systemic inflammation and joint pain reveals the interconnected roles of the gut, mitochondria, and nervous system in driving chronic discomfort and fatigue. Understanding this cellular and neural cross-talk provides a more complete, functional framework for recovery.

- Published on Oct 27th, 2025
Table of Contents
Let’s talk about joint pain. If you’ve ever dealt with aching joints, you’ve probably been told it’s just wear and tear. But what if that’s not the whole story? What if that pain is actually a message? What if that pain is a signal from the body indicating that something deeper is going on?
The key insight here is to stop staring only at the joint, the knee, shoulder, or wrist, and start looking at the underlying reason for the pain. The body is sending out an SOS signal, not random noise. It’s communicating that the internal environment is under stress.
A Systemic SOS Signal:
Why Joints Send a Message
From a clinical standpoint, this distress often occurs at the cellular level, involving what can be described as cellular distress and defensive overdrive, cells struggling to survive while defense systems remain locked in the “on” position (Hotamisligil, 2017 PubMed).
Research shows that these dysfunctions can originate in the gut, immune system, and nervous system, with the joint merely serving as the visible alarm.
Inflammation Cascade:
When Healing Harms
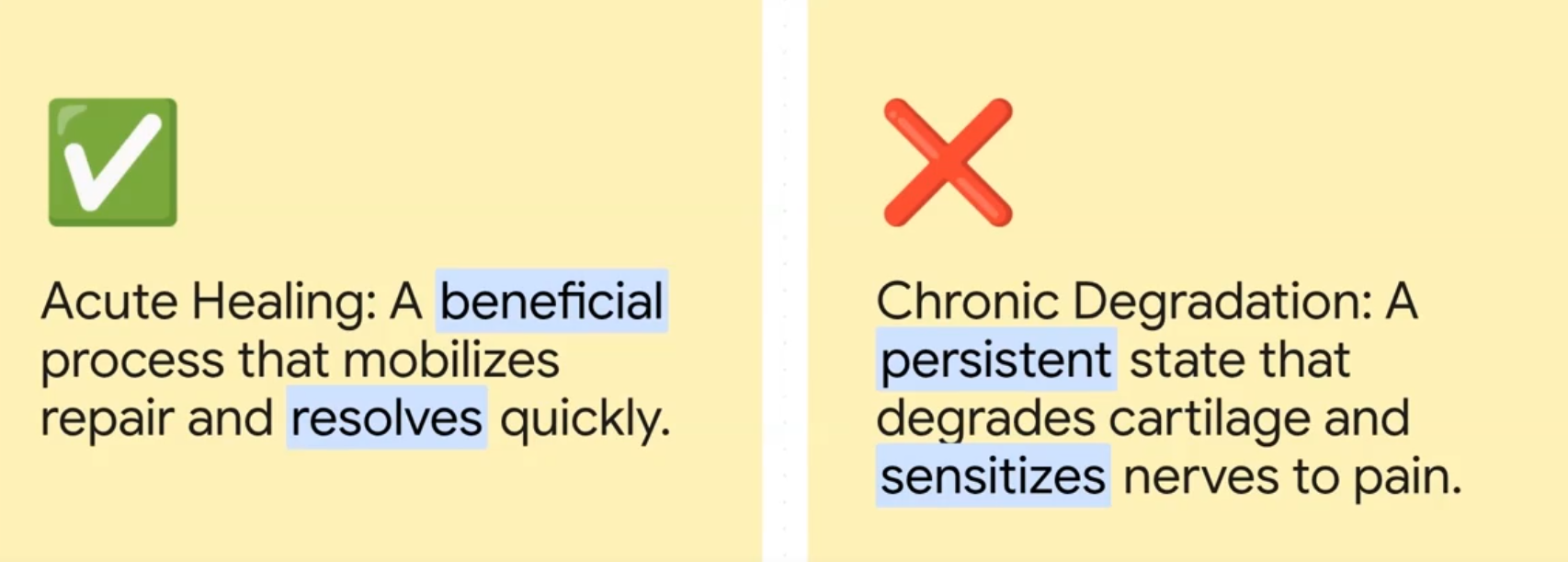
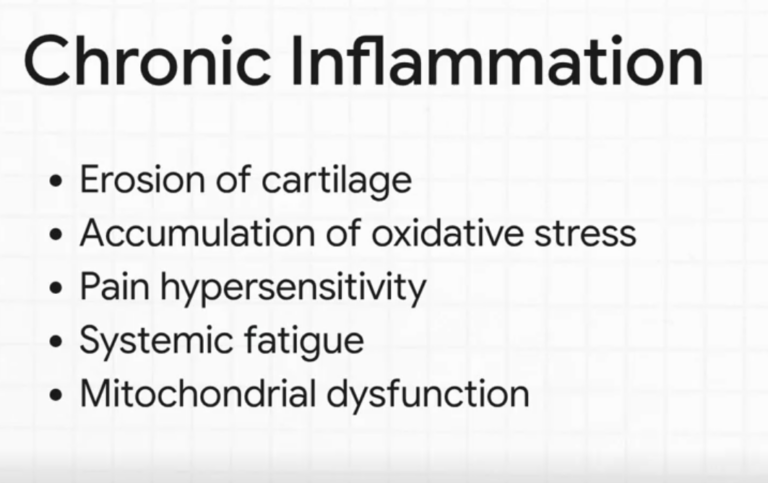
Central to this entire cascade is inflammation. Acute inflammation is beneficial and necessary for healing (Medzhitov, 2008 PubMed). However, when this process becomes chronic, it transitions from protection to self-damage, contributing to cartilage degradation and pain hypersensitivity (Hunter & Felson, 2006 PubMed).
This chronic inflammatory state generates oxidative stress, effectively creating a “rusting” process within cells. It heightens nerve sensitivity and spreads systemically, leading to fatigue and mitochondrial dysfunction (Murphy, 2009 PubMed).
Unmasking Root Causes:
Tracing Pain to its Source
To understand why this happens, it’s essential to trace the cascade backward to its sources. Let’s look into this below.
The first is gut permeability (“leaky gut”) which allows antigens to cross into circulation, triggering immune confusion and auto-reactivity that can target joint tissue (Fasano, 2012 PubMed).
Mitochondrial dysfunction is what impairs cellular energy production, limiting repair and promoting fatigue.
We must also consider metabolic and stress-related factors such as glycation from unstable blood sugar, nutrient deficiencies, and chronic psychological stress. All of which further aggravate inflammation and collagen stiffness (Brownlee, 2001 PubMed)
When Pain Gets Stuck:
The Brain's Role
Another crucial dimension involves central sensitization, where pain persists even after tissue healing. Here, the brain itself becomes overreactive, continuing to generate pain despite the absence of active injury (Woolf, 2011 PubMed). This maladaptive neural loop represents the nervous system’s “alarm” stuck in overdrive.
The 3-Phase Healing Path:
Roadmap to Recalibration
As joint pain reflects systemic dysregulation, the solution must also be systemic.
A functional recovery roadmap unfolds in three phases:

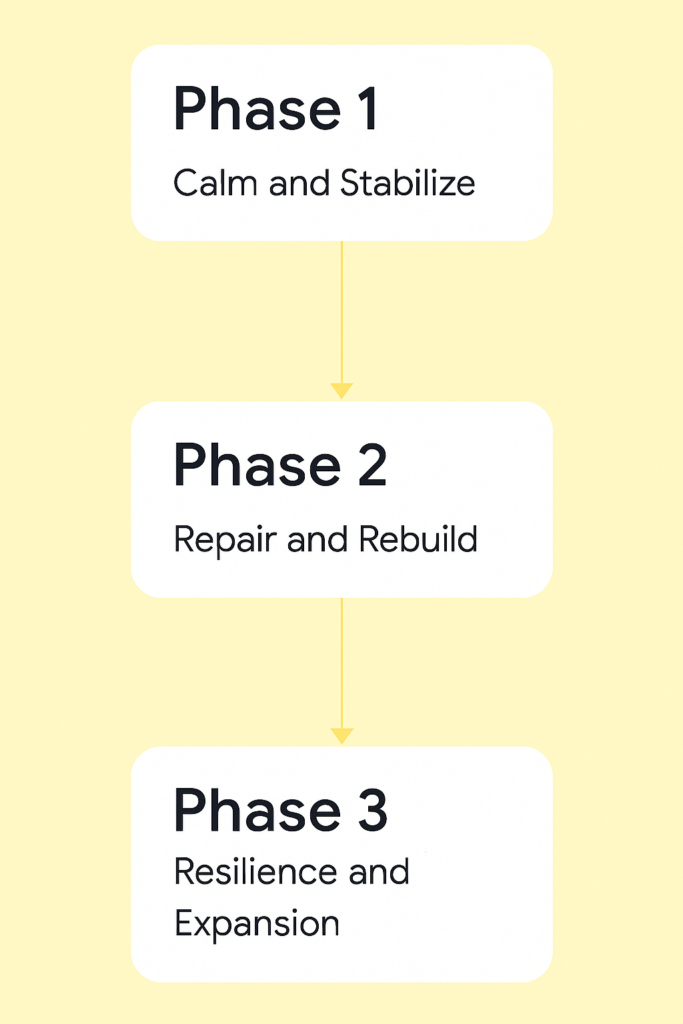
- Calm the system – When the nervous system is dysregulated, it’s necessary to decrease inflammatory inputs, support gut integrity, and engage limbic system retraining through breathwork and mindfulness to reduce neural threat signals.
- Repair and rebuild – Once the system is calmed, we must restore mitochondrial efficiency with nutrients such as thiamine and magnesium, and use gentle movement to nourish joints and reinforce parasympathetic activity.
- Resilience and reintroduction – We can then begin to rebuild strength and metabolic flexibility through structured training and emotional stability, promoting long-term adaptability.
Ultimately, real recovery from chronic joint pain arises not from silencing symptoms but from understanding the message the body is sending.
This is how pain becomes a signal for recalibration; it’s an invitation for systemic repair and restoration.
If you are experiencing joint pain, these signs are telling you that something deeper is going on. We see this often at the Integrated Health Foundation. Many of our clients experience joint pain, some have a diagnosis, and some do not. You can find out more about how we work with our clients with symptoms just like joint pain by clicking here, or see below to take our free Symptoms Evaluation Assessment.
Do You Have Dysautonomia?
Take our quick and comprehensive symptom assessment to find out if your symptoms align with dysautonomia and receive personalized insights.
Frequently Asked Questions
What causes chronic joint pain beyond wear and tear?
Chronic joint pain often reflects systemic inflammation involving the gut, immune, and nervous systems rather than isolated joint degeneration.
How is inflammation linked to joint damage?
Persistent inflammation triggers oxidative stress and cartilage breakdown, sensitizing nerves and amplifying pain perception.
Can gut health influence joint pain?
Yes. Increased intestinal permeability allows immune activation that can target joint tissues, a mechanism described in autoimmune-related arthritis.
What role do mitochondria play in joint health?
Mitochondria provide energy for tissue repair. Dysfunctional mitochondria contribute to both fatigue and degeneration of joint structures.
Why does pain persist even after tissue healing?
Central sensitization in the brain can maintain pain signals independent of ongoing tissue injury.
What strategies help regulate chronic joint pain?
Calming inflammation, restoring gut integrity, supporting mitochondrial function, and retraining the brain’s pain response form the foundation.
Is joint pain reversible?
With systemic regulation, targeting inflammation, energy metabolism, and neural sensitization, many forms of chronic joint pain can significantly improve.
Read More Articles

Vertigo: Why the Nervous System Causes Chronic Dizziness (POTS, Dysautonomia, Chronic Illness)
Vertigo is not simply a balance problem, it’s a sign of deeper physiological dysregulation involving the vestibular system, blood flow, gut-brain axis, and stress response. This article explores how inflammation, posture, and autonomic imbalance contribute to dizziness and offers insight into restoring internal balance.
Why You Can’t “Just Calm Down”: Chronic Anxiety (It’s Not Just In Your Head!)
Chronic anxiety is more than an emotion, it’s a full-body state of dysregulation involving the nervous system, mitochondria, and stress hormones. Learn how overactive brain circuits, gut imbalance, and energy metabolism interact to sustain anxiety, and how retraining the body restores calm regulation.

Explaining Palpitations
Heart palpitations can feel sudden and alarming, yet they usually arise from the body’s regulation systems, not from heart disease. This article explores how stress, posture, breathing, hydration, minerals, and gut health affect rhythm and reveal the body working to stay balanced.
Temperature Sensitivity
Many people struggle with feeling too hot or too cold when others feel fine. This article explores how the autonomic nervous system, cellular energy, and inflammation control internal temperature and why these systems can fall out of balance.

Why Your Hands Get Freezing Cold
Cold hands and feet often reflect more than poor circulation, they’re signals from the nervous system. This article explains how vasoconstriction, stress, and autonomic imbalance redirect blood flow and what that reveals about the body’s intelligent protective mechanisms.

The Biology of Hopelessness
Hopelessness is not a personal failure but a biological state driven by chronic stress and nervous system overload. When survival mode dominates, the amygdala, stress hormones, and energy systems shift, suppressing motivation and perspective. Understanding this physiology creates a clear path toward restoration.

