What is a Dysregulated Nervous System? | IHF

Written by Scott Pringle, Founder of the Integrated Health Foundation
- Published on July 20th, 2025
- If you prefer not to read the article or have screen sensitivity, you may listen to this audio version

Table of Contents
- What is a Dysregulated Nervous System?
- Common Symptoms of Autonomic Nervous System Dysfunction
- The Science Behind Your Symptoms
- The Connection Between Chronic Illness and Dysregulated Nervous System Symptoms
- Natural Ways to Repair Your Autonomic Nervous System
- When to Seek Professional Help
- Your Roadmap to Recovery
What is a Dysregulated Nervous System?
If you’ve ever felt wired yet exhausted, struggled to calm down no matter how hard you try, or wondered why your body seems stuck in fight-or-flight mode, you’re not alone. Many people don’t realize they may have a Dysregulated Nervous System. The state where your body’s autopilot settings are constantly firing when they shouldn’t.
When your nervous system is dysregulated, daily life can feel like an uphill battle. Sleep doesn’t refresh you, stress feels impossible to shake, and your body may react with weird, unexplained symptoms.
But here’s the good news: once you understand what nervous system dysregulation is, you can learn to work with your body instead of fighting against it.
In this article, we’ll break down what a dysregulated nervous system really means, what causes it, how to spot the signs, and most importantly what you can do today to start the healing process naturally.
That being said, let’s consider some aspects of how the nervous system can behave when regulated. The best way to help individuals understand this is to think of the nervous system as preset programs that run automatically.
These programs run on routine schedules, and they run all the processes in the body. You don’t have to think about these programs like you would to stretch your muscles or run a race. Instead, they happen unconsciously.
It is very important that they run in harmony and coordinate, and articulate information back and forth between other bodily systems.
Like a computer that runs programs, if something happens where a program becomes corrupted or damaged in some way, the time frames or the signals for those programs can begin running errors, or as we like to call it, become dysregulated. The automatic functions become affected and irregular.
So what could that look like?
Let’s consider a system of the body, like the cardiovascular system.
This system is in charge of things like: the heart muscle and the frequency of heartbeats per minute, the pressure of the blood as it’s pumped through the body, the strength of the heart and its ability to pump blood from the feet and back to the head, etc.
If this program were to become dysregulated, then the heart rate could become erratic, it could pump too fast or too slow, it could react to stimuli in a paradoxical way, or in an opposite way than it should. One of the ways we see this is with POTS. Patients here fall under the umbrella of dysautonomia and dysregulated nervous system patients. The program that runs the system of the cardiovascular circuit is dysregulated. Hence, the symptoms that the patient will feel are dizziness or lightheadedness when their blood pressure is abnormal; they may have high or low blood pressure at the wrong time, or they may have very high heart rates at a time when they shouldn’t. Blood may also pool in their feet as their blood vessels are not able to push the blood back to the heart fast enough. Nothing is actually damaged or injured in the situation, there is simply a dysregulation in the normal programming that runs the cardiovascular system.
If you experienced POTS, what would you feel as symptoms?
Well, your heart might race for no reason, you could feel dizzy when you stand up, or constantly exhausted despite getting enough sleep.
Basically, a dysregulated nervous system occurs when your autonomic nervous system, the command center that controls your unconscious bodily functions, isn’t working properly.
The autonomic nervous system (ANS) is responsible for regulating not just random functions of the body, but the most crucial ones. We already discussed the heart rate and blood pressure, but there are more systems that control other uniting systems of the body, like the digestive system, sympathetic/parasympathetic (fight or flight), circadian rhythm (sleep cycles), and temperature regulation.
A thing as simple as your body shifting its temperature down in a hot room becomes an impossible task, or it can become an exertion of the hypothalamus to overcorrect, and you become too cold. It’s like having a faulty thermostat in your home, things either run too hot or too cold and finding balance becomes nearly impossible.
See how these dysregulation systems can really put a damper on a typical activity?
It’s this dysregulation that can trigger a cascade of seemingly unrelated symptoms that many doctors struggle to connect, leaving patients frustrated and searching for answers.
Scientific Note: These changes have been observed in clinical research. For example, a review in Frontiers in Integrative Neuroscience emphasized how both chronic stress and inflammation contribute to functional reorganization of the autonomic nervous system, reinforcing the idea that these “software errors” can cause wide-ranging physiological disruptions.
At the Integrated Health Foundation, we understand this frustration all too well. Millions of Americans are living with dysregulated nervous system symptoms, many without a proper diagnosis or effective treatment options.
The good news? Understanding these symptoms is the first step toward recovery.
Common Symptoms of Autonomic Nervous System Dysfunction
In his Substack article “Postural Orthostatic Tachycardia Syndrome (POTS),” Dr. Peter McCullough links the spike protein from both SARS-CoV-2 infection and mRNA vaccination to disruptions in the autonomic nervous system. He describes how the spike protein appears to damage small nerve fibers that regulate heart rate and vascular tone, leading to conditions like POTS. He emphasizes, “The disaggregation of the autonomic nervous system explains the profound exercise intolerance and tachycardia many patients experience after vaccination or COVID-19.”
While McCullough’s Substack claims are not peer-reviewed, there is growing academic evidence supporting this phenomenon. For instance, peer-reviewed research has confirmed the occurrence of small fiber neuropathy and autonomic dysfunction in both post-COVID and post-vaccine individuals. A study published in Nature Reviews Cardiology found cardiovascular autonomic dysfunction in up to 30% of symptomatic long-term COVID patients, consistent with McCullough’s clinical observations.
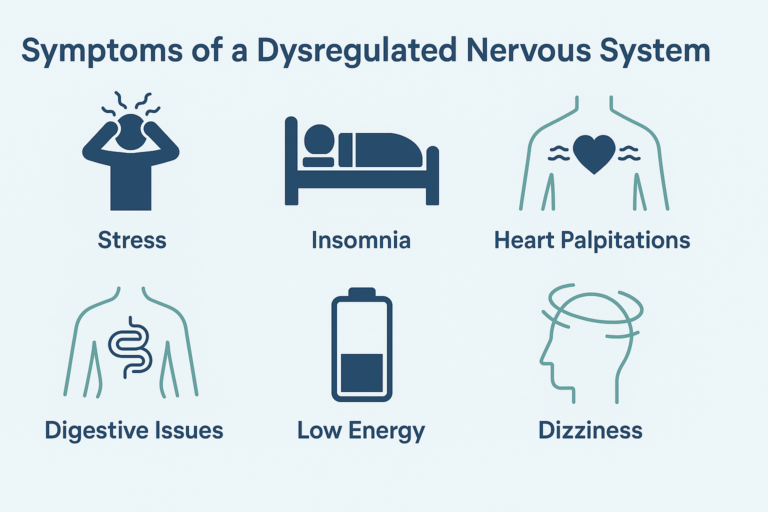
When your nervous system is dysregulated, it can manifest in numerous ways throughout your body. Dysregulated nervous system symptoms can range from mild inconveniences to debilitating conditions that significantly impact your quality of life. Here are some of the most common signs that your autonomic nervous system might be struggling:
Cardiovascular System
This is often the most noticeable. You might feel your heart pounding or racing (especially when you stand up), get lightheaded or dizzy, or even pass out. Blood pressure may swing too low or too high for no reason.
- Rapid heartbeat or palpitations, especially when changing positions
- Blood pressure fluctuations (either too high or too low)
- Poor circulation results in cold hands and feet
- Light-headedness or dizziness upon standing
Digestive System
Your gut can slow down or speed up unpredictably, causing nausea, bloating, constipation, diarrhea, or a heavy, full feeling even when you haven’t eaten much.
- Unpredictable bowel movements
- Nausea after eating
- Excessive gas or bloating
Feeling full quickly
Respiratory System
Some people feel short of breath or like they can’t get a deep enough breath, even though their lungs and oxygen levels are technically fine.
- Air hunger or shallow breathing
- Feeling breathless under minor exertion
Urinary and Reproductive Systems
Bladder issues like frequent urgency, leakage, or trouble emptying are common. Sexual function can also be disrupted, including low libido or arousal problems.
- Frequent urination or urgency
- Incontinence or retention
- Reduced sexual desire or arousal
Temperature and Sweat Regulation (Thermoregulatory System)
You might sweat too much or not at all, feel hot when everyone else is fine, or get chilled easily. It’s like your internal thermostat stops working.
Unexplained temperature shifts
Excessive or insufficient sweating
Intolerance to heat or cold
Night sweats
Ocular System
Trouble adjusting to light or darkness, blurry vision, or sensitivity to brightness can all stem from nervous system issues affecting the eyes.
- Light sensitivity
- Blurred vision in varying light
- Difficulty focusing
Endocrine and Metabolic Systems
Hormones can go out of sync, leading to blood sugar crashes, low energy, or symptoms that feel like adrenal burnout, especially under stress.
- Blood sugar irregularities
- Persistent fatigue despite sleep
- Salt or sugar cravings
Neurological System
Brain fog, difficulty concentrating, anxiety, and even panic attacks can be part of the picture. It’s not “just in your head”—your nervous system is out of balance.
- Difficulty concentrating
- Sudden anxiety or panic
- Emotional reactivity
- Sleep disturbances
These overlapping symptoms, across so many body systems, are not coincidental. Autonomic dysfunction is increasingly understood as a systemic issue with complex feedback loops between the brain, immune system, and cardiovascular regulation. In fact, research from Nature Medicine has shown that COVID-19 survivors have a higher risk of long-term neurological issues, including dysautonomia, than the general population.
Many people experiencing these dysregulated nervous system symptoms have been told their problems are “all in their head” or given vague diagnoses without effective treatment options. But these symptoms are very real and often stem from measurable dysfunction in the autonomic nervous system.

The Science Behind Your Symptoms
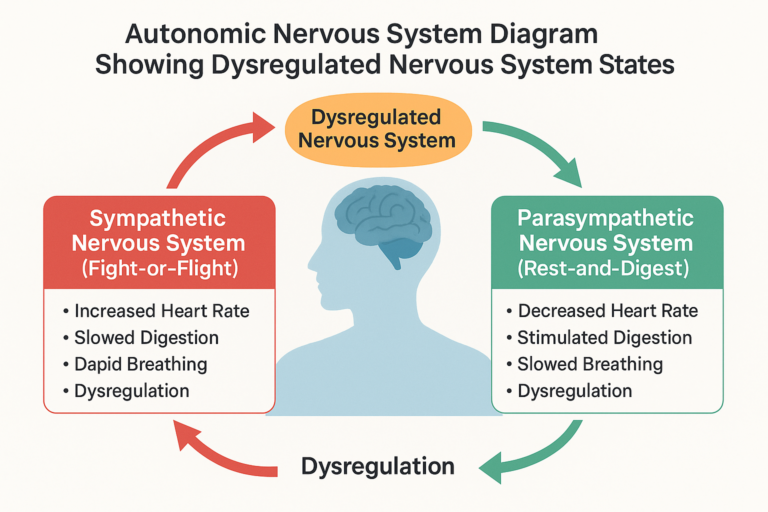
To understand dysregulated nervous system symptoms, we need to look at the two main branches of the autonomic nervous system: the sympathetic (“fight-or-flight”) and parasympathetic (“rest-and-digest”) nervous systems.
In a healthy individual, these two systems work in harmony. The sympathetic system activates during times of stress or danger, while the parasympathetic system takes over during periods of rest and recovery. This delicate balance ensures that your body can respond appropriately to different situations while maintaining overall homeostasis.
However, chronic stress, illness, trauma, or genetic factors can disrupt this balance. When your sympathetic nervous system becomes stuck in the “on” position, your body remains in a constant state of high alert. This persistent fight-or-flight response can deplete your resources and lead to many of the dysregulated nervous system symptoms mentioned above.
Conversely, some individuals experience parasympathetic dominance, where the body struggles to mobilize appropriate energy when needed. This can result in extreme fatigue, low blood pressure, and digestive slowdown.
What’s happening in both of these scenarios is essentially a programming error within the body’s automatic systems. This dysfunction isn’t always visible through standard tests, which is why many patients go undiagnosed for months or years. But just because the dysfunction is “invisible” doesn’t mean it isn’t real.
Scientific Corroboration
Research shows that people suffering from autonomic dysregulation often exhibit clear physiological markers. For example, heart rate variability (HRV) (a measure of how well the nervous system adapts to stress) tends to be significantly lower in these individuals. Lower HRV is a sign that the body is locked in a sympathetic-dominant state, unable to switch gears and recover effectively.
Similarly, abnormal cortisol rhythms and elevated inflammatory cytokines like IL-6 and TNF-alpha have been linked with chronic nervous system dysregulation. These biomarkers are especially pronounced in patients with long COVID, chronic fatigue syndrome, and fibromyalgia.
Additionally, brain imaging studies have shown that persistent sympathetic activation may physically alter the brain. Regions like the hypothalamus, amygdala, and prefrontal cortex (all heavily involved in autonomic regulation) can show signs of structural and functional change in those with long-standing dysregulation.
This helps explain why people with dysregulated nervous systems often feel “stuck” in patterns of exhaustion, overwhelm, or hypersensitivity. The neural circuits themselves are functioning differently.
Post-COVID Impact
After COVID-19, more clinicians are recognizing dysautonomia as a key driver of lingering symptoms. In fact, recent reviews in journals such as Frontiers in Medicine and Nature Reviews Cardiology suggest that many post-viral syndromes—including long COVID—should be viewed through the lens of autonomic nervous system disruption.
As one large-scale study from Nature Medicine (2022) concluded:
“There is a markedly increased risk of autonomic, cardiovascular, and neurological dysfunction at 12 months following acute COVID-19—even in individuals with mild or asymptomatic cases”.
These aren’t imaginary problems, they’re physiological responses to a system that’s struggling to maintain balance. And while conventional medicine may not always recognize this type of dysfunction, modern neuroscience and cardiology are beginning to catch up.
Understanding this science is crucial and not just to validate your experience, but to guide the right interventions. This is a huge part of our ethos at the Integrated Health Foundation. We believe that knowledge is power, once you understand the ‘why’ behind your symptoms, you can begin to piece together the ‘what’ is required for recovery,
The Connection Between Chronic Illness and Dysregulated Nervous System Symptoms

Many chronic conditions have autonomic dysfunction at their core, even though conventional medicine often treats them as separate entities. Dysregulated nervous system symptoms frequently appear in:
Autoimmune Disorders:
Conditions like Hashimoto’s thyroiditis, lupus, and rheumatoid arthritis often involve autonomic disruption as either a cause or effect of the immune dysfunction. Research has shown that the inflammatory cytokines released during autoimmune flares can interfere with vagal tone and sympathetic-parasympathetic balance.
Fibromyalgia and Chronic Fatigue Syndrome (CFS/ME):
These conditions are increasingly recognized as manifestations of central nervous system sensitization and autonomic imbalance. Studies show that individuals with fibromyalgia often present with impaired heart rate variability and altered baroreflex sensitivity, both signs of nervous system dysregulation.
POTS and Dysautonomia:
Postural Orthostatic Tachycardia Syndrome (POTS) is a form of dysautonomia characterized by an abnormal increase in heart rate upon standing, along with numerous other dysregulated nervous system symptoms. POTS diagnoses have surged since COVID-19, especially among young women, with researchers estimating that up to 30% of long COVID patients may meet criteria for POTS.
Mast Cell Activation Syndrome (MCAS):
This condition involves inappropriate mast cell activation and can both contribute to and result from autonomic dysregulation. MCAS symptoms, ranging from flushing and hives to gastrointestinal upset and palpitations, often overlap with ANS dysfunction, particularly in the context of long COVID or Lyme disease.
Post-Viral Syndromes:
Following infections like mononucleosis, Lyme disease, or COVID-19, many patients develop persistent dysregulated nervous system symptoms as part of their recovery process. This pattern has been particularly evident since the COVID-19 pandemic, with numerous studies documenting long-lasting cardiovascular, neurological, and autonomic symptoms in survivors, even those with mild initial illness.
“In long COVID, dysfunction of the autonomic nervous system appears to be a common denominator across multiple organ systems.”
— Nature Reviews Cardiology, 2023
Understanding this connection is crucial because treating the underlying autonomic dysfunction can often improve seemingly unrelated symptoms. Rather than managing each symptom individually with different medications, addressing the root cause—the dysregulated nervous system—may provide more comprehensive relief.
In fact, clinicians who take an integrative approach are increasingly using autonomic testing as part of their diagnostic toolkit for patients with persistent, unexplained symptoms. Heart rate variability (HRV), tilt-table tests, and symptom clusters have become important clues in identifying underlying nervous system imbalance.
As we continue to see the ripple effects of COVID-19 and chronic inflammatory diseases on autonomic function, it’s becoming more apparent that nervous system health is central, not peripheral, to many forms of chronic illness.
How to Heal a Dysregulated Nervous System Naturally
If you’re experiencing dysregulated nervous system symptoms, there are several evidence-based approaches that can help restore balance. These techniques focus on supporting your body’s natural regulatory mechanisms rather than simply masking symptoms.

Breathing Techniques:
Conscious breathing practices like diaphragmatic breathing, box breathing, and alternate nostril breathing can directly activate your parasympathetic nervous system, helping to counteract stress responses. Regular use of these techniques has been shown to lower cortisol levels, stabilize heart rate variability (HRV), and reduce anxiety in individuals with autonomic dysfunction.
Vagus Nerve Stimulation:
The vagus nerve is the main highway of your parasympathetic nervous system. Simple techniques like humming, gargling, cold water face immersion, or specialized massage can stimulate this nerve and promote regulation. Non-invasive vagus nerve stimulation (nVNS) is currently being explored as a therapeutic tool for POTS, fibromyalgia, and PTSD, with promising early results.
Movement Therapies:
Gentle, mindful movement practices such as yoga, tai chi, and qigong can reset dysfunctional nervous system patterns. Unlike high-intensity exercise (which can sometimes worsen dysregulated nervous system symptoms), these approaches focus on creating safety signals for your ANS. A meta-analysis published in Frontiers in Psychology found that movement therapies not only reduced sympathetic arousal but also improved HRV and emotional resilience in patients with chronic illness.
Sleep Hygiene:
Quality sleep is essential for nervous system repair. Establishing consistent sleep routines, creating a cool, dark sleeping environment, and limiting screen exposure before bedtime can significantly improve autonomic function. Studies show that even one night of poor sleep can lead to elevated sympathetic tone and reduce parasympathetic recovery responses the following day.
Mindfulness and Meditation:
Regular mindfulness practice has been shown to reduce sympathetic activation and increase parasympathetic tone, helping to balance the autonomic nervous system over time. In fact, long-term meditators often show higher baseline HRV—a sign of robust autonomic adaptability.
A Note on Consistency:
Healing a dysregulated nervous system takes time and consistency. Small, sustainable changes often yield better results than dramatic interventions that can’t be maintained. Even five minutes of breathwork, gentle stretching, or mindful silence each day can begin to reprogram the nervous system toward safety and stability.
As with any chronic condition, tracking your symptoms and progress is essential. Tools like HRV monitors, symptom journals, and guided recovery programs can help reinforce your body’s capacity for healing.
When to Seek Professional Help
While self-help strategies can be incredibly effective for managing dysregulated nervous system symptoms, certain situations warrant professional support.
At the Integrated Health Foundation we have a team of experts who facilitate weekly support calls working with an integrated protocol which is tailored to the unique condition of the individual.
What kind of practitioner should you look for?
Seek out providers who understand the bidirectional relationship between the brain and body. Those who recognize how trauma, infection, environment, and inflammation interact with autonomic regulation.
Practitioners versed in integrative cardiology or neuroimmune modulation are especially well-equipped to handle these overlapping systems. At the Integrated Health Foundation we emphasize whole-person recovery strategies grounded in neuroscience, immunology, and cardiovascular medicine.
When your nervous system is dysregulated, your entire experience of life can shift. Professional support is not a sign of weakness—it’s an acknowledgment that this is a complex physiological issue, deserving of thoughtful, personalized care.
Your Roadmap to Recovery
Recovering from dysregulated nervous system symptoms isn’t always linear, but having a structured approach can make the journey less overwhelming. Here’s a basic roadmap:
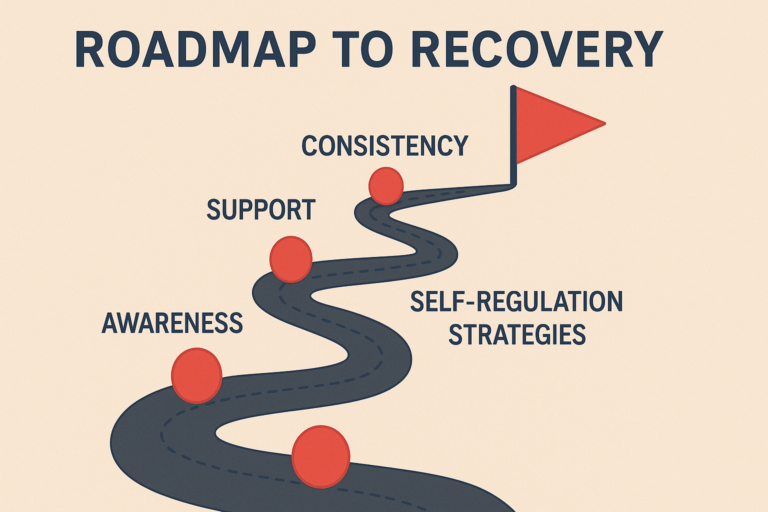
1. Assessment and Understanding
Begin by identifying your specific dysregulated nervous system symptoms and potential triggers. Our Symptoms Evaluation Assessment can help you gain clarity about what’s happening in your body. This is more than symptom-checking, it’s pattern recognition. Looking at how your digestive issues might line up with fatigue, or how your sleep problems flare after stress, is the first step to revealing the nervous system’s fingerprints across your health.
2. Create Safety for Your Nervous System
Before introducing significant changes, focus on establishing basic nervous system “safety.” This could be as simple as improving your sleep hygiene, drinking more water with electrolytes, or doing short breathing exercises daily. Your nervous system can only heal when it feels safe. If it’s constantly scanning for threats, whether emotional, environmental, or inflammatory, it will resist regulation. Research shows that polyvagal-informed practices such as social connection, eye contact, and rhythmic movement can promote this sense of physiological safety.
3. Track Patterns and Progress
Use a journal or app to track symptoms, energy levels, stress exposure, and even weather or hormonal changes. Dysregulated systems are often cyclical and flare-prone. Noticing patterns can help prevent crashes and guide future interventions. Tools like heart rate variability (HRV) monitors, pulse oximeters, or even simple symptom checklists can provide measurable feedback over time.
4. Address Deeper Roots
In many cases, especially those involving long COVID, autoimmune flares, trauma, or chronic infection, professional testing may reveal deeper imbalances. These might include immune dysregulation, gut microbiome imbalances, adrenal fatigue, or mitochondrial dysfunction. A qualified integrative or neuroimmune practitioner can help you interpret this data and tailor treatment accordingly.
5. Rebuild Resilience
Eventually, recovery moves beyond symptom management into resilience building. This means expanding your nervous system’s capacity to handle life’s stressors (both internal and external) without spiraling into dysregulation. This phase often includes cognitive retraining, social re-engagement, movement reconditioning, and long-term stress inoculation techniques.
“Nervous system resilience is not just about feeling calm. It’s the ability to experience a challenge and return to equilibrium efficiently.”
— Frontiers in Integrative Neuroscience, 2023
6. Stay Connected and Supported
Healing your Dysregulated Nervous System is a communal process. Isolation fuels sympathetic overdrive. Having practitioners, friends, support groups, or spiritual practices that foster trust and co-regulation is essential. Loneliness, in fact, has been shown to activate the same brain areas as physical pain, and can derail progress if left unaddressed.
At the Integrated Health Foundation we understand the importance and value of community, especially when dealing with dysregulation in isolation. For many of our clients, the community becomes not only their number one support network, but it becomes like a second family.
FAQs About Dysregulated Nervous System
A dysregulated nervous system happens when your body’s stress response is stuck in overdrive. This can lead to chronic fight-or-flight or freeze states, making it hard to feel calm and safe.
Causes include chronic stress, past trauma, ongoing inflammation, poor sleep, and nervous system disorders like POTS or dysautonomia.
Yes! With daily practices like breathwork, gentle movement, nutrition, and regulating your stress, many people can gradually rebalance their nervous system naturally.
Signs include better sleep, feeling calm more often, less reactivity to stress, improved digestion, and more stable energy throughout the day.
Everyone’s timeline is different. It can take weeks to months of consistent practice, depending on stress levels, lifestyle, and your body’s history.
A dysregulated nervous system doesn’t mean you’re broken, it means your body needs help finding safety again. By recognizing the signs, understanding the root causes, and trying simple daily tools, you can gently guide your nervous system back to balance.
Healing doesn’t happen overnight, but every small step counts. Listen to your body, get curious about what soothes you, and remember: you’re not alone!
If you think you might have a dysregulated nervous system, take our free Symptoms Assessment today. Start your journey toward a calmer, more resilient you.
Evaluate Your Symptoms: Do You Have Dysautonomia?
Take our quick and comprehensive symptom assessment to find out if your symptoms align with dysautonomia and receive personalized insights.
Share This Article
Read More Articles

Is Your Nervous System Overmedicated or Under supported?
Calm your overactive nervous system naturally: root causes, real healing tools & steps to feel safe again. Take our free assessment today!

What is the Carnivore Diet: Benefits, Risks, and Science Explained
Explore the Carnivore Diet: benefits, risks & real results for chronic illness. Take our free health assessment today!
What treatment options are available for dysautonomia?
Dysautonomia is a condition where there is a dysfunction in the autonomic nervous system (ANS) which controls unconscious body functions such as breathing, blood pressure,

