
Table of Contents
- Understanding Nervous System Dysfunction
- Types of Nervous System Dysfunction (Parasympathetic vs Sympathetic)
- Underlying Mechanisms of Nervous System Imbalance
- How Nervous System Malfunction Affects Body Systems
- The Hyperactive Autonomic Nervous System Explained
- Nervous System Disorders Comparison
- What Would Happen if the Nervous System Stopped Working
- Frequently Asked Questions About Nervous Dysfunction
Are you experiencing unexplained symptoms that doctors can’t seem to pinpoint?
A dysfunction of nervous system might be at the root of your health struggles.
This comprehensive article explores nervous system imbalance, its various manifestations, and why understanding this complex system is crucial for those dealing with mysterious chronic conditions.
Understanding Nervous System Dysfunction
Imagine your body as a sophisticated city with an intricate network of communication lines. The nervous system functions as both the electrical grid and the telecommunications network, sending critical messages that keep everything functioning smoothly.
Let’s take the term ‘dysfunction’, defined as ‘a problem or fault in a part of the body or a machine’.
When a dysfunction of nervous system occurs, it’s like experiencing power outages or crossed wires in different parts of the city.
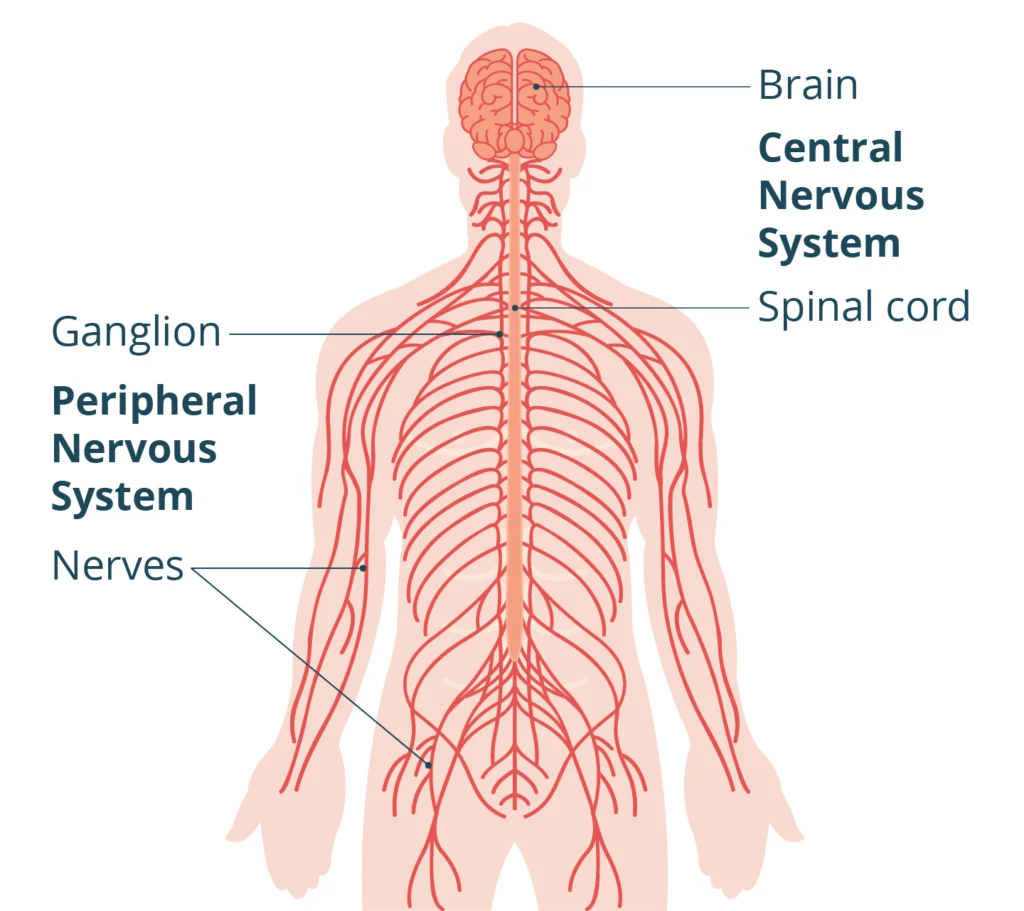
Nervous system dysfunction refers to improper functioning of any part of this complex network, including the brain, spinal cord, or peripheral nerves. This dysfunction can affect virtually every aspect of your well-being, from basic bodily functions to complex cognitive processes.
Unlike obvious injuries or illnesses, nervous dysfunction often manifests as a collection of seemingly unrelated symptoms that can be frustratingly difficult to diagnose.
What makes nervous system dysfunction so challenging?
For many people, the struggle isn’t just physical, it’s the maddening experience of knowing something is wrong while medical tests come back “normal.” This disconnect between lived experience and clinical findings leaves many feeling invalidated and desperate for answers.
At the Integrated Health Foundation, we recognize this struggle and understand that nervous system imbalance requires a comprehensive, individualized and whole-person approach.
Types of Nervous System Dysfunction (Parasympathetic vs Sympathetic)
Your autonomic nervous system (the automatic control center for vital functions) consists of two primary branches that should work in harmony: the sympathetic and parasympathetic nervous systems. Understanding the balance between these systems is essential for grasping how a dysfunctional nervous system impacts your health.

Sympathetic Dysfunction
The sympathetic nervous system governs your “fight-or-flight” response. When functioning properly, it activates during stress or emergencies, increasing heart rate, dilating pupils, and redirecting blood flow to muscles.
When the body is in sympathetic dysfunction:
- Your body may remain in a constant state of high alert
- Stress responses activate with minimal or no actual threats
- Recovery becomes difficult even in safe environments
This overactivation leads to what many experience as feeling “wired but tired”, exhausted yet unable to relax. Have you ever felt your heart racing while trying to fall asleep, despite being physically exhausted? This paradoxical state often indicates sympathetic dominance.
Parasympathetic Dysfunction
Conversely, the parasympathetic system manages “rest-and-digest” functions, promoting recovery, digestion, and tissue repair. Parasympathetic dysfunction can manifest as:
- Digestive disturbances despite healthy eating habits
- Poor recovery from minor exertions
- Difficulty transitioning to restful states, even when tired
- Compromised immune function
Understanding the balance between these systems is crucial for comprehending how nervous system dysfunction impacts overall health. When one system becomes dominant or dysfunctional, it can lead to a range of symptoms affecting multiple body systems.
The Dysfunction Spectrum
Rather than distinct categories, most people with nervous system imbalance experience a spectrum of dysfunction, with one system potentially overactive and the other underresponsive. This creates a complex range of manifestations that can shift and change depending on stressors, environmental factors, and internal biochemistry.
Underlying Mechanisms of Nervous System Imbalance
What causes a normally functioning nervous system to become dysfunctional?
Several interrelated mechanisms contribute to this malfunction of nervous system:
Inflammation and the Nervous System
Chronic inflammation (whether from infection, environmental toxins, or internal stressors) can directly impact neural function. Inflammatory cytokines alter the way nerves transmit signals and can damage the protective coating around nerve fibers called myelin. This process creates a negative feedback loop: inflammation disrupts nervous function, which then signals more inflammation.
This means that essentially, when parts of your body stay swollen for a long time from things like germs, pollution, or stress, it can mess up the way your nerves talk to each other and hurt their protective covers, which can make the swelling even worse.
Inflammatory Triggers Include:
- Chronic infections (including stealth infections like Epstein-Barr virus)
- Environmental toxins and heavy metals
- Food sensitivities and gut dysfunction
- Physical trauma, including seemingly minor injuries
- Psychological stress and trauma
Autonomic Dysregulation
The autonomic nervous system requires precise regulation. When this balance falters, a cascade of dysfunction follows. Common dysregulation patterns include:
- Hypersensitive Threat Detection: The amygdala, a key structure in the brain’s limbic system, plays a crucial role in processing emotional events and threat detection. In individuals with dysautonomia, the amygdala may become overly responsive to potential threats. This hypersensitivity can lead to increased anxiety and exaggerated stress responses, even in non-threatening situations.
- Impaired Vagal Tone: The vagus nerve is a primary component of the parasympathetic nervous system. Dysfunction in vagal tone can result in various symptoms, including digestive disturbances, heart rate irregularities, and difficulty with the “rest-and-digest” functions.
- Altered Baroreceptor Sensitivity: Baroreceptors are sensors that monitor blood pressure and play a crucial role in maintaining cardiovascular homeostasis. Disruption in baroreceptor sensitivity can contribute to orthostatic intolerance, a common symptom in dysautonomia characterized by dizziness, lightheadedness, and fainting upon standing
- Sympathetic Dominance: Chronic activation of the sympathetic nervous system, even in non-threatening situations, is a hallmark of many autonomic disorders. This can manifest as persistent tachycardia, hypertension, excessive sweating, and other symptoms associated with a prolonged “fight-or-flight” state.
These dysregulation patterns can interact and reinforce each other, creating a complex clinical picture. For example, hypersensitive threat detection may lead to increased sympathetic activation, which in turn can further impair vagal tone and baroreceptor function.
Understanding these mechanisms is crucial for developing targeted interventions and managing the diverse symptoms associated with autonomic dysregulation.
Mitochondrial Impact
Our mitochondria, our cellular energy producers, are highly sensitive to nervous system signals. When nervous system dysfunction persists, mitochondrial function suffers, creating an energy crisis at the cellular level. This explains why fatigue is often a predominant feature in those with autonomic dysfunction. A study published in Nature Communications by Monash University researchers highlighted how neuronal signals, particularly involving neurotransmitters like GABA and acetylcholine, regulate mitochondrial stress responses and maintain energy production across tissues.
Think of mitochondria as tiny batteries inside your cells that give you energy. They listen to signals from your brain to work properly. When your nervous system isn’t working well, those signals get mixed up, and the batteries can’t charge as they should. This makes you feel really tired because your body doesn’t have enough energy.
HPA Axis Connection
The hypothalamic-pituitary-adrenal (HPA) axis forms a critical communication network between the brain and adrenal glands. Nervous system dysfunction alters this communication, disrupting stress hormone regulation.
Over time, this contributes to what’s commonly described as “adrenal fatigue,” though the root problem often begins with nervous system imbalance. A study published in Molecular Systems Biology introduced a model showing how prolonged stress dysregulates the HPA axis by altering gland mass dynamics and feedback mechanisms. This dysregulation can lead to chronic stress-related disorders such as anxiety, depression, and fatigue.
The HPA axis is like a team of messengers in your body that helps you deal with stress. When you’re stressed, it sends signals to release special hormones like cortisol to give you energy and keep you alert. But if your nervous system keeps telling it there’s danger when there isn’t, the messengers get confused and work too hard. Over time, this can make you feel really tired and stressed out all the time.
How Nervous System Malfunction Affects Body Systems
The ripple effects of nervous system dysfunction extend throughout the body, explaining the constellation of symptoms that often appear unrelated in conventional medicine. Many patients report seeking answers for these symptoms, only to be offered treatments targeting individual issues in isolation, rather than considering the body as a whole.

Cardiovascular Effects
Your heart and blood vessels rely on precise nervous control. When this control falters:
- Heart rate irregularities (e.g., tachycardia) can occur due to autonomic dysregulation (source).
- Blood vessel dysfunction leads to improper constriction or dilation, causing blood pooling or inadequate circulation (source).
- Blood pressure regulation issues, such as orthostatic intolerance, can result from baroreceptor sensitivity disruption (source).
- Chest pain or discomfort may arise without evidence of cardiac disease due to autonomic dysfunction (source).
“Many patients diagnosed with anxiety are actually experiencing cardiovascular manifestations of autonomic dysfunction,” notes cardiologists specializing in dysautonomia.
Digestive System Disruption
The enteric nervous system—often called the “second brain”—governs digestive function and is heavily influenced by the autonomic nervous system. Dysfunction manifests as:
- Irregular motility, leading to symptoms such as diarrhea or constipation (source).
- Altered enzyme production, impairing digestion and nutrient absorption (source).
- Disrupted gut barrier function, which may increase intestinal permeability and inflammation (source).
- Gut microbiome imbalances, contributing to symptoms resembling IBS or SIBO (source).
Immune System Consequences
Your nervous system directly communicates with immune cells, influencing their activity. When this communication becomes dysfunctional:
- Heightened inflammatory responses occur, worsening autoimmune tendencies (source).
- Natural killer cell function diminishes, reducing the immune system’s ability to fight infections (source).
Allergic and sensitivity reactions often increase due to immune dysregulation (source).
Endocrine System Effects
Hormone production and regulation depend on proper nervous system signaling. Dysfunction creates:
- Thyroid imbalances despite normal lab values, often due to disrupted hypothalamic-pituitary signaling (source).
- Sex hormone fluctuations, which can lead to reproductive issues (source).
- Insulin resistance and metabolic disturbances caused by autonomic dysregulation (source).
- Disrupted circadian hormone patterns affecting sleep and energy regulation (source).
Neurological Impacts
Perhaps most distressing are the neurological manifestations of nervous system dysfunction:
- Brain fog: impaired concentration, memory issues, and cognitive slowness (source).
- Sensory sensitivity: heightened reactions to light, sound, smell, and touch (source).
- Pain perception changes: increased pain sensitivity or unusual pain patterns due to disrupted nerve signaling (source).
- Sleep disturbances: difficulty falling asleep, staying asleep, or achieving restful sleep caused by autonomic imbalance (source).
- Mood alterations: anxiety, depression, irritability, or emotional instability resulting from nervous system dysregulation (source).
The Hyperactive Autonomic Nervous System Explained
A hyperactive autonomic nervous system represents a common pattern of dysfunction where the body’s automatic control systems become overly responsive to stimuli that should normally be filtered or moderated.
Signs of Hyperactive Autonomic Function:
- Exaggerated startle response
- Difficulty filtering background stimuli
- Sensory overwhelm in busy environments
- Disproportionate physiological responses to minor stressors
- “Crashes” after seemingly normal activities
Imagine your body has a control center that manages things like your heartbeat and breathing without you having to think about it. Sometimes, this control center can become too sensitive, like when the volume on a TV is turned up too high. This makes everything feel louder and more intense, even things that shouldn’t bother you much.
A hyperactive autonomic nervous system can be likened to having the volume turned up too high on all sensory and internal inputs. The world becomes overwhelming because the system can’t properly filter and prioritize incoming information.
The Freeze Response
While “fight-or-flight” is commonly discussed, many with hyperactive autonomic function experience a “freeze” response—a shutdown mode that occurs when the system becomes overwhelmed. This manifests as:
- Sudden fatigue or “hitting a wall”
- Brain fog descending rapidly
- Difficulty speaking or finding words
- A need to withdraw from stimulation
- Temporary cognitive impairment
Sometimes, when your body’s control center gets too overwhelmed, it might suddenly make you feel very tired or confused. It’s like when a computer freezes because too many programs are running at once. This isn’t because you’re lazy or don’t want to do things; it’s your body’s way of trying to protect itself when everything feels too much.
This response often confuses both patients and practitioners, as it appears to come on suddenly and can be mistaken for laziness, lack of motivation, or psychiatric issues. In reality, it’s a protective mechanism when the nervous system becomes overloaded.
Physical Symptoms of an Overactive Nervous System:
- Digestive distress like acid reflux, nausea, or irritable bowel, which can be linked to an overactive sympathetic nervous system causing digestive problems.
- Frequent headaches and body aches, often associated with sympathetic overdrive.
- Disrupted sleep cycles and constant fatigue, which are common in cases of autonomic hyperactivity.
- Rapid heart rate, palpitations, or chest pain, indicative of sympathetic hyperactivity.
- Low immunity with recurrent illnesses, which can result from chronic stress responses mediated by the sympathetic nervous system.
Emotional Symptoms:
- Anxiety and restlessness, often linked to an overactive nervous system.
- Chronic stress, which can lead to sympathetic dominance.
- Emotional instability, which may be exacerbated by autonomic hyperactivity.
- Difficulty concentrating, which can be a result of sympathetic overactivity.
Understanding these symptoms can help both patients and healthcare providers recognize and address hyperactive autonomic function more effectively.
It’s important to remember that these responses are not a sign of weakness, but rather a physiological reaction to an overactive nervous system. These responses are very familiar to us and the clients we work with.
Let’s explore this further and take a look at comparing different categorized nervous system disorders.
Nervous System Disorders Comparison
Understanding how nervous system dysfunction relates to diagnosed conditions can help contextualize your experience:
| Condition | Primary Systems Affected | Diagnostic Approach | Connection to Nervous Dysfunction |
| Fibromyalgia | Central nervous system, muscles | Clinical criteria, ruling out other conditions | Often involves central sensitization and autonomic imbalance |
| ME/CFS | Multiple systems including immune, autonomic, and central nervous system | Clinical criteria, exclusion of other causes | Strongly linked to autonomic dysfunction and impaired stress recovery |
| POTS (Postural Orthostatic Tachycardia Syndrome) | Autonomic control of heart rate and blood pressure | Tilt table test, standing test | Direct manifestation of autonomic dysfunction affecting cardiovascular control |
| MCAS (Mast Cell Activation Syndrome) | Immune system, specifically mast cells | Chemical mediator testing, response to treatment | Mast cells are directly influenced by nervous system signals |
| Hashimoto’s Thyroiditis | Thyroid gland | Antibody testing, thyroid function tests | Autonomic function affects thyroid hormone conversion and receptor sensitivity |
What’s crucial to understand is that these conditions often overlap and share a common thread of nervous system involvement. Rather than viewing them as distinct diseases, many practitioners now see them as different manifestations of similar underlying dysfunction.
This is why at the Integrated Health Foundation, we don’t address only individualized symptoms or diagnosis. We get to the root cause of what has occurred in the body to date, to then understand what is needed to pave the path towards remission by looking at the body as a whole.
What Would Happen if the Nervous System Stopped Working
While complete nervous system failure is incompatible with life, understanding the consequences of progressive dysfunction illuminates why addressing nervous system health is critical.
Critical Functions Under Nervous Control
As we know by now, the nervous system regulates several vital functions:
- Breathing regulation: Controls rhythm, depth, and responsiveness to CO2 levels
- Heart function: Coordinates heart rate, contractions, and blood pressure
- Temperature regulation: Maintains internal body temperature
- Digestion coordination: Manages movement of food, enzyme release, and nutrient absorption
- Immune surveillance: Detects and responds to pathogens
- Conscious thought: Processes information, manages memory, and controls cognitive function
- Movement control: Governs fine motor skills and basic coordination
The Domino Effect of Dysfunction
As nervous system function declines, a predictable pattern emerges and can be broken down into the following stages:
- Early stage: Subtle symptoms often attributed to stress or aging
- Fatigue
- Mild memory issues
- Slight coordination problems
- Intermediate stage: Clear dysfunction in multiple systems with significant quality of life impact
- Digestive issues
- Sleep disturbances
- Mood changes
- Cognitive decline
- Advanced stage: Profound disability with severe limitations
- Significant motor control loss
- Severe cognitive impairment
- Major organ system dysfunction
Hope for Recovery
The good news is that this progression can often be halted or even reversed when the underlying dysfunction is properly addressed. The body possesses remarkable neuroplasticity (the ability to rewire and heal neural pathways) when given the right support, which is exactly why we offer up to 7 weekly support calls in our core program at the Integrated Health Foundation.
Frequently Asked Questions About Nervous Dysfunction
What damages the nervous system in the first place?
The autonomic nervous system can be damaged or dysregulated by:
- Chronic stress and trauma
- Viral and bacterial infections
- Autoimmune conditions
- Genetics
- Lifestyle factors (poor diet, lack of physical activity, inadequate sleep)
- Underlying health conditions
- Adverse childhood experiences (ACEs)
Research has shown that chronic stress, trauma, and adverse childhood experiences are significant contributors to nervous system dysregulation.
No, they are different. Neurological diseases usually involve identifiable damage or degeneration of nervous tissue. Nervous system dysfunction refers to improper function that may occur without visible structural damage. However, if left unaddressed, prolonged dysfunction could potentially lead to structural changes.
While chronic stress is a significant contributor to nervous system dysfunction, most cases involve multiple factors. These may include:
- Infections
- Environmental toxins
- Genetic predispositions
- Physical trauma
Stress often acts as the “final straw” that overwhelms the body’s adaptive capacity.
Consider these questions:
- Do your symptoms affect multiple body systems?
- Do symptoms worsen with stress and sensory overload?
- Have conventional treatments provided limited relief?
- Do you experience good days and bad days without clear triggers?
- Have you been told your tests are normal despite significant symptoms?
If you answered yes to several of these questions, nervous system dysfunction may be contributing to your condition.
Rather than thinking in terms of “cure,” consider the concept of recovery and resilience. The nervous system is remarkably adaptable, and many people achieve significant improvement or complete resolution of symptoms with proper support. The journey is often non-linear, with progress occurring in waves rather than a straight line.
Treatment approaches may include:
- Lifestyle modifications (diet, exercise, sleep hygiene)
- Stress reduction techniques (meditation, yoga, deep breathing exercises)
- Targeted nutritional support
- Physical therapy or occupational therapy
- Cognitive behavioral therapy
- In some cases, medication to manage specific symptoms
The most effective treatment plans are typically personalized and address multiple aspects of health simultaneously.

Conclusion: Finding Your Path Forward
Understanding nervous system dysfunction opens new possibilities for those struggling with chronic, complex conditions. Rather than treating isolated symptoms, addressing the root dysfunction can create fundamental shifts in health and well-being.
At the Integrated Health Foundation, we recognize the profound impact of nervous system imbalance and the frustration many feel when conventional approaches fall short. Our approach integrates cutting-edge science with practical, personalized strategies to support nervous system regulation and resilience.
Ready to explore whether nervous system dysfunction might be at the root of your health challenges? Our comprehensive Symptoms Evaluation Assessment can help identify patterns that point to autonomic imbalance and create a clearer picture of your unique situation.
Take our Symptoms Assessment Today and take the first step toward understanding and addressing the root causes of your health concerns.
Evaluate Your Symptoms: Do You Have Dysautonomia?
Take our quick and comprehensive symptom assessment to find out if your symptoms align with dysautonomia and receive personalized insights.
Share This Article
Read More Articles

Is Your Nervous System Overmedicated or Under supported?
Calm your overactive nervous system naturally: root causes, real healing tools & steps to feel safe again. Take our free assessment today!

What is a Dysregulated Nervous System?
Discover what a dysregulated nervous system is, explore symptoms & recovery options, and take our free Symptoms Assessment today!

What is the Carnivore Diet: Benefits, Risks, and Science Explained
Explore the Carnivore Diet: benefits, risks & real results for chronic illness. Take our free health assessment today!


